Nature has come up with a million ways to get us sick, and we’ve cured only a tiny fraction of them. From common flus and infections, to epidemics and superbugs, to the unexpected downsides that come with increased life expectancy, medical researchers and biotechnology experts have plenty of work to do.
Luckily, San Diego County is home to a world-class cluster of universities, medical research and health care institutes, and biotech and pharmaceutical companies. The variety within our life sciences industry ensures that anyone seeking solutions for fundamental and applied research, drug discovery and development, clinical trials, or bringing treatments to market never has too far to look.
Many local biotech leaders are long-established heavyweights, but genetic sequencing, genomics, and the medical device and diagnostic sectors have seen especially rapid growth in recent years, thanks in part to the emergence of CRISPR gene editing technology and digitally enabled medicine. Here, we take a look at of some of the most promising research and breakthrough discoveries happening right in our own backyard.

Zika and Malaria
Everyone hates mosquitoes—some scientists have even proposed “gene drives” to engineer them to resist parasites like malaria, or to eliminate the ones that spread Zika and dengue fever entirely. San Diego researchers are now at work on less controversial yet still-effective methods to fight such diseases.
Malaria remains one of the world’s most deadly contagious diseases. The World Health Organization estimates that half of all humans on earth are at risk of dying from it. Over 200 million people get it every year, and it kills over half a million people annually, especially children under 5. Population growth, resilient mosquitoes, and donor fatigue—in which financial help slowly dries up due to chronic need or a perceived lack of progress—make the problem even more challenging. Despite some progress and the expanded use of drugs and insecticide-treated bed nets, no vaccine fully protects against malaria.
“What we’d really like to do is to think about getting rid of malaria once and for all in the next 30 years,” says Elizabeth Winzeler, a microbiologist at UC San Diego. “But we need completely new approaches and next-generation medicines to eliminate all stages of the parasite.”
200 million Malaria cases appear annually
These protozoa kill over 500 thousand people every year
One mosquito bite releases 100 parasites into your blood
The Bill and Melinda Gates Foundation awarded Winzeler’s research team nearly $5 million last year to develop therapies to eventually eradicate the disease. The team is taking a two-pronged approach: They’re searching for drug targets and Achilles’ heels in every part of the malaria parasite’s life cycle, and, using research inspired by work on HIV, they’re working to develop new drugs that could be used like a chemical vaccine and formulated to be delivered to people at risk.
Just one mosquito bite can introduce 100 parasites into your body. By the time they reach your bloodstream, they’ve grown a thousandfold; once you have a fever, you’ve got a billion parasites swarming around and the damage is done. “We want to tackle it early on, before the infection develops,” Winzeler says. “Then you might not need as much of the drug around, and the potential for resistance is lower.”
Viruses, like Zika and dengue, pose different problems. Someone with Zika might show only a few symptoms, or symptoms easily mistaken for a flu, making it hard to diagnose before it spreads. The disease also spreads from mother to child in the womb, sometimes causing microcephaly, in which the infant is born with a smaller head and brain. The rate of new infections has declined, but it, too, could have a resurgence.
“We’d like to get rid of malaria once and for all in the next 30 years … but it’s very difficult to find a silver bullet.”
Gene Tan and Brett Pickett of the J. Craig Venter Institute have been gathering hundreds of Zika samples from around the world, mainly from Central and South America and the United States, and sequencing various types to better understand its genome.
Tan is finishing up a project to figure out how Zika’s antibodies work and what mechanisms determine how they can stop the virus. Tan and Pickett are also trying to identify which proteins are modified during a Zika infection and how they can be targeted. By developing their genomic sequencing tools and diagnostic methods, they want to play their part to improve public health.
“A lot of pharmaceutical companies, and even us, we’re trying to make a collective contribution to the scientific community,” Tan says. “It’s very difficult these days to find a silver bullet.”
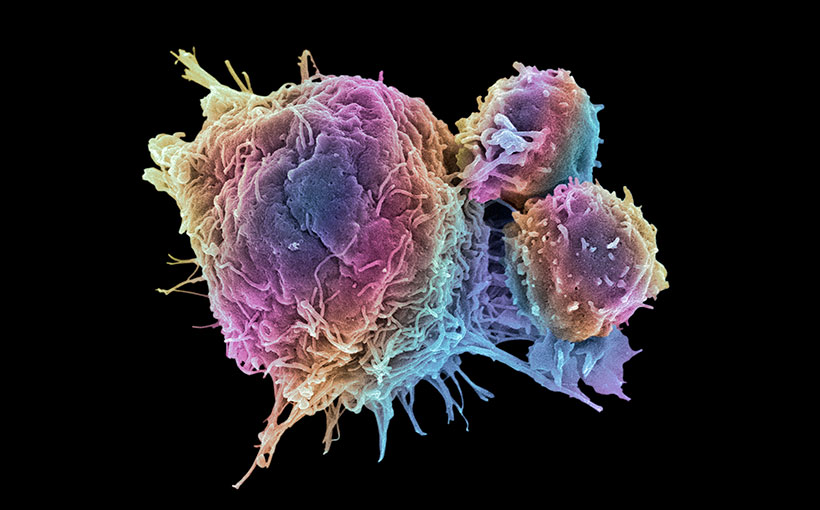
Cancer
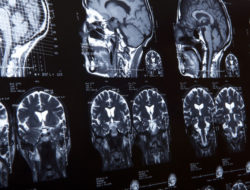
Cancer surpassed heart disease in 2016 as the leading cause of death in California, according to the Centers for Disease Control and Prevention. Brain cancer isn’t as common as breast, prostate, or lung cancer, but it’s far more lethal. Brain tumors vary so much that no two look the same, and it’s impossible to develop a drug target for every kind of mutation or every route for the cell signals that might be involved.
Frank Furnari, a researcher at the Ludwig Institute for Cancer Research, now has the ability to build different types of brain tumors from normal human stem cells, put them into mice, then see how they vary and evolve. He has merged two technologies to do this: modifiable stem cells and the powerful gene-editing tool CRISPR-Cas9. He hopes to find some commonality to brain tumors, despite the great variance of their genetic makeups.
2018 will see an estimated 1,735,350 new cancer cases
16,830 people will die from brain and spinal cord tumors this year
A man’s lifetime cancer diagnosis probability is 39.7 percent. It’s only slightly less for women.
Source: American Cancer Society
With personalized cancer medicine, scientists look at a patient’s genotype and try to develop a therapy tailored to them. But it turns out that tumors evolve as you treat them, which poses an additional problem, according to Paul Mischel, also of the Ludwig Institute. “We found that tumors do change, and the rate at which this was happening was way faster than anyone would expect,” he says. This makes it harder to spot the cells with genes predisposed to cause cancer. When a brain tumor forms, it rapidly evolves and can quickly become dangerous and resistant to drugs used to treat it.
Mischel and his colleagues have also found that the most important genes driving cancer are no longer just chromosomal—many of them have jumped to DNA outside the cell nucleus and have become mobile. They also drive the variation in tumors, making patients more vulnerable and the tumors all the more complicated to study and treat.
“I think this is a paradigm shift,” Mischel says. “This is fundamentally changing the biology of these tumors.”
The average life expectancy of someone with brain cancer, even with aggressive chemotherapy and surgery, is currently just 14 months. “We want to make a difference and extend the lives of these patients,” Furnari says.
Diabetes
Nearly one-tenth of Californian adults have been diagnosed with diabetes, and many more have blood sugar levels high enough to put them at risk of it. That means that some 300,000 people in San Diego County are diabetic, and probably 5 to 10 percent of those—about 20,000—have Type 1, in which their pancreas can’t make insulin and their body can’t regulate their blood sugar, which can be devastating.
“These insulin therapies have to outsmart the host’s immune system, which would otherwise destroy the new cells.”
With $14 million from JDRF and $72 million more from the California Institute for Regenerative Medicine, San Diego-based ViaCyte is working on clinical trials of its stem-cell-derived therapy for Type 1 diabetes.

“We have all the tools necessary for treating diabetes and delivering these products to patients,” says Paul Laikind, ViaCyte’s president and CEO. Their researchers have developed a cell therapy platform called PEC-Encap, which uses stem cells to make pancreatic cells within an implantable device that resembles a tea bag.
These therapies have to outsmart the host’s immune system, which would otherwise destroy the new insulin-producing cells, so they designed PEC-Encap with a semipermeable membrane that lets insulin through but keeps well-meaning immune cells out. Another approach, called PEC-Direct, is intended for high-risk patients. It requires immune suppression medications; without an immune response to worry about, it allows blood vessels to connect directly to the cells inside the device. It’s the furthest along—already in clinical trials—putting the company ahead of competitors like Encellin in San Francisco.
1.5 million Americans are diagnosed with diabetes every year
Diabetes is the seventh leading cause of death in the United States
Around 300,000 people in San Diego County are diabetic
Source: American Diabetes Association
For the next generation of treatment, ViaCyte is using gene editing techniques to make the stem-cell line unrecognizable to the body. If the immune system doesn’t perceive those cells as foreign, treatment becomes easier and more flexible. “It’s an exciting area,” Laikind says. “We think the industry will move in that direction.”
Genetic Conditions
Meanwhile, researchers throughout San Diego are making progress on mapping, sequencing, editing, and probing the workings of the human genome.
Gene Yeo, a cellular and molecular scientist at UC San Diego, has modified CRISPR-Cas9 to edit not just DNA but also RNA, the messenger molecule that controls how genes are turned on and off and how proteins form. His team is using this new system to correct certain molecular defects and mutations. In particular, they seek to stop anomalously repeating RNA sequences that, when left unchecked, can lead to Lou Gehrig’s disease and Huntington’s disease. Yeo and his colleagues launched a new San Diego biotech company, Locana, to focus on these diseases and bring the technology to the clinic.
At the Salk Institute, a team of scientists led by Juan Carlos Izpisua Belmonte has made their own modified version of CRISPR-Cas9. The original tool works by making “double-strand breaks” in DNA in particular places, but this can produce unwanted mutations at the targeting site, so its precision is less than ideal. Izpisua Belmonte and his team adapted the tool to operate without making these breaks, and they demonstrated that it could be used to treat diseases like diabetes and muscular dystrophy in mice.
“The technique took four years to develop, and in the beginning, it was quite a struggle to get it to work efficiently,” says Hsin-Kai (Ken) Liao, first author of the study. “We want to go from mice to nonhuman primates, and our ultimate goal is to help patients, especially for incurable age-related diseases.” That includes Alzheimer’s and Parkinson’s.
Proteins regulate our genetic material, too. They’re not just inert blobs in a cell; they interact with and modify other proteins, and some parts of them may be more important to those interactions than previously thought.
“I think on the surfaces of proteins, there’s this vast regulatory network we haven’t yet probed,” says Vicki Lundblad, a molecular and cell biologist at Salk. “We can find evidence for it and we can pinpoint it down to a couple amino acids.”
She and her colleagues uncovered the role of protein surfaces by accident, while sifting through 300,000 yeast cells. They plan to study drug targets on particular locations of protein surfaces, which could eventually lead to new cancer therapies.

Impending Disruption
Fundamental research and the patient-facing application of that research often occur in completely different places. The Scripps Research Institute tries to bridge that chasm by guiding inventions and discoveries in microbiology, chemistry, and neuroscience as directly as possible into medicines and diagnostics.
For example, osteoarthritis, a joint disease that afflicts tens of millions of Americans, often requires knee replacements in patients over 60. TSRI researchers have developed a regenerative therapy consisting solely of injections, and now that same institute is putting it into a clinical setting. The therapy is designed to stimulate the body’s existing stem cells to re-create knee joint cartilage.
Health care will be disrupted. It will come from the patient, who will be empowered.”
Matt Tremblay is the vice president of business development at TSRI. He’s also chief operating officer of Calibr, a spinoff company that has since been reintegrated into Scripps. While a typical university might receive a 2 percent royalty on drugs developed by its researchers, Calibr gets up to 10 percent. But TSRI remains a nonprofit, as that extra financial support is channeled back into research. It also offsets the currently unpredictable amount of federal funding they can expect from agencies like the National Institutes of Health and the National Science Foundation.
“We’re now plugged into the technology coming from Scripps,” Tremblay says. “We shepherd them along, find partnerships, and move them faster toward impacting patients. We conduct the clinical trials ourselves, which is pretty unprecedented for a research institute or university to do.”
He believes the future of precision medicine will involve more app-enabled health, in which people monitor and quantify their health with consumer electronic devices like smart watches. People can report their own health stats with them more frequently than they visit the doctor, potentially facilitating more appropriate treatments. The downsides of these new tools—among them privacy concerns, and a potential rise in hypochondria—will of course deserve continuing scrutiny.
An estimated 30.8 million adults have osteoarthritis
65 percent of patients with osteoarthritis are prescribed NSAIDs
172 million work days are lost each year due to arthritis and other rheumatic conditions
Source: Arthritis Foundation
Larry Smarr, director of the Qualcomm Institute, agrees with these predictions. In recent years he has come to quantify every aspect of his health on a daily basis—or even more frequently. Despite a normal-looking colonoscopy, his self-recorded health information helped lead his doctors to the discovery of his inflammatory bowel disease before it became too dangerous.
“I think health care will be disrupted,” Smarr says, “and I think it will come from the patient, who is going to be empowered with more capable devices that generate all this data, and more of the data will be shared in the cloud, and then artificial intelligence will be able to give you individual feedback. While it’s not a doctor, it’s there every second of every day.”
Tags: Biotech, Cancer, Health, Medical Research, Medicine, Zika Virus